Osteochondrosis is the cause of acute back pain in 67% of all cases. Lack of timely consultation with a doctor, advice and treatment can lead to consequences such as dysfunction of internal organs, damage to the spinal cord and damage to the nerve roots of the spine. What is osteochondrosis, what treatment options are available for patients and how is the disease diagnosed – read on.
What is Osteochondrosis?

Osteochondrosis is a degenerative-dystrophic disease that leads to thinning of the intervertebral cartilage. Hyaline cartilage and intervertebral discs begin to "wear out" and lose their full functionality.
Reference.In most cases, spinal osteochondrosis is diagnosed in people aged 25 and over. According to the WHO, in 2021, 43% of the population aged 25 to 40 suffers from osteochondrosis, of which more than 92% of people are aged. The occurrence and exacerbation of the disease can be caused by unfavorable environmental factors.
Types of osteochondrosis
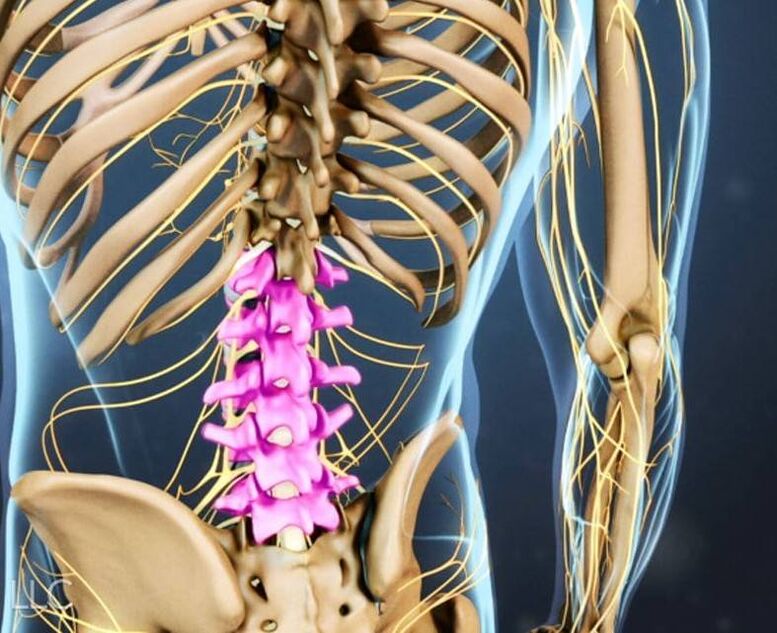
Every part of the spine is subject to degeneration processes. Among the types of osteochondrosis of the spine, three main types can be distinguished: cervical, thoracic and lumbar (due to the high load it is more common than others).
- Lumbar osteochondrosis.The lumbar region consists of 5 vertebrae, which are subject to deformation due to the negative effects of external and internal factors. When nutritional and metabolic processes in the intervertebral discs are disrupted, pain occurs, which is caused by loss of elasticity and thinning of cartilage tissue.
- Cervical osteochondrosis.The cervical spine consists of 7 vertebrae that are regularly exposed to stress. Pathological processes are activated when the body's metabolic processes fail.
- Breast osteochondrosis.The thoracic region consists of 12 vertebrae. This type of osteochondrosis is the least common. The thoracic vertebrae are inactive. People who lead a passive lifestyle and regularly lift heavy objects are susceptible to the disease.
Causes of osteochondrosis
The number of people suffering from osteochondrosis is growing rapidly every year. This is because people spend most of their time on their feet, putting maximum strain on the intervertebral discs.
Important!With increasing age or due to heavy stress, intervertebral discs and cartilage deform. Clefts and hernias may occur. The result is compressed nerve roots, thinned intervertebral discs, pathological processes in the spinal cord, muscle spasms and progressive pain.
The risk group includes: office workers, construction workers, hairdressers, salespeople, drivers. Both men and women are equally susceptible to the occurrence of osteochondrosis.
The provoking factors of osteochondrosis include:
- Presence of osteochondrosis in the family history;
- overweight, obesity;
- passive lifestyle;
- Flat feet.
Impaired depreciation of the spine and its deformation can be caused by the following factors:
- Self-neglect (complete lack of physical activity or excessive exercise).
- Lack of awareness of proper posture to reduce stress on the spine.
- Constant work that involves lifting/moving heavy objects.
- Injuries.
Osteochondrosis: 4 stages of disease development

There are 4 stages of development of spinal osteochondrosis:
- First stage– There are no clear symptoms by which the disease can be diagnosed. Back pain occasionally occurs, often after physical exertion or overexertion. Osteochondrosis in the early stages can be detected during a preventive examination or during a CT or X-ray examination.
- Second floor.The next stage is characterized by moderate pain. The cartilage tissue begins to deform and the distance between the intervertebral discs decreases. When contacting a doctor, drug therapy (to relieve pain) and physiotherapy are prescribed.
- Third section– The spine is deformed, fibrous spots and hernias appear, the pain increases and becomes more pronounced and frequent. At this stage everything depends on the symptoms present. The doctor helps determine the method of treatment for the patient (conservative or surgical).
- Fourth stage– irreversible deformation of spinal function. It is almost impossible for the patient to move independently. The pain is acute, constant and increases with any physical activity. Pathological bone tissue fills the intervertebral space and the patient becomes disabled.
Symptoms of osteochondrosis
As already mentioned, there are three types of osteochondrosis, each of which is characterized by individual manifestations. Let's take a closer look at all the symptoms.
Symptoms of lumbar osteochondrosis
How do you know if you have lumbar osteochondrosis? You may notice characteristic symptoms:
- stiffness of movements;
- Pain in the pelvis, sacrum, lower back and lower extremities that increases with exercise or movement. The nature of the pain is aching, dull, sharp;
- pathological processes of the urogenital system (problems with bowel movements and urination);
- weakness in legs;
- Impairment/lack of sensitivity.
Important!Self-medication is strictly prohibited. If lumbar osteochondrosis is detected, diagnosis and effective treatment are mandatory. The consequences of a lack of therapy are hernias, bulges and paralysis of the lower extremities.
Symptoms of cervical osteochondrosis

How do you know if you have cervical osteochondrosis? One or more symptoms may occur:
- regular headaches;
- numbness of upper and lower extremities;
- severe crunching in the cervical spine during physical activity;
- "spots", spots in the eyes, clouding and darkening;
- burning and discomfort in the heart area;
- the appearance of tinnitus, hearing loss;
- causeless dizziness;
- Pain in shoulders, neck, arms.
Important!Osteochondrosis of the cervical spine is considered one of the most dangerous for humans, as it complicates the process of blood saturation of the brain. If left untreated, protrusions and then hernias appear. Surgical intervention for cervical osteochondrosis carries a high risk of paralysis of the body. If symptoms occur, contact only qualified personnel.
Symptoms of thoracic osteochondrosis

How do you know if you have thoracic osteochondrosis? Only a doctor (neurologist) can diagnose the disease, but the patient may assume the presence of osteochondrosis based on characteristic signs:
- malaise, a burning feeling in the chest;
- the appearance of pain when raising your arms, pain in the shoulder blades;
- Dizziness and sudden loss of consciousness occur;
- Chest pain.
Reference.As the disease transitions into the acute phase, dorsalgia (lack of air, stabbing/stiff chest pain, "lumbago") and dorsalgia (pain can be episodic or constant, acute/dull in nature) may occur.
Osteochondrosis of the thoracic spine is difficult to diagnose. The disease is often confused with angina pectoris, a heart attack or inflammatory processes in the lungs.
Diagnosis of spinal osteochondrosis
The medical history and physical examination of the musculoskeletal system begins when you visit the doctor.
Patient's device. The specialist checks the integrity of reflexes and the sensitivity of painful areas. Blood tests and other laboratory tests will then be ordered. To clarify the diagnosis, the neurologist prescribes one or more types of imaging diagnostics:
- Ultrasound of the vertebral arteries.
- X-ray of the entire spine or specific areas (cervical, thoracic, lumbar spine).
- A CT scan of the spine helps to detect degenerative processes, displacements and deformations of the spine and its structures.
- MRI of the spine – identifies soft tissue pathologies and helps scan the spinal cord and intervertebral discs.

Treatment of osteochondrosis
How to treat osteochondrosis is determined by the attending physician depending on the type of disease, the severity of the symptoms and the degree of pathological changes. The following can be used as therapeutic therapy: physiotherapy, drug treatment, courses at the chiropractor, therapeutic massage, exercise therapy or surgical intervention (in the absence of positive dynamics from other treatment methods or in an advanced stage).
Drug treatment of osteochondrosis
When prescribing drug therapy, the doctor may use several groups of drugs at once:
- NSAIDs (non-steroidal anti-inflammatory drugs) – used to relieve the symptoms of osteochondrosis, relieve pain and reduce inflammation. Can be used in tablet form or as an injection (in severe cases). The duration of treatment is 7 to 14 days;
- Chondroprotectors – to strengthen the intervertebral discs and cartilage tissue;
- B vitamins;
- Vascular medications – to improve blood supply to the spine;
- Glucocorticosteroids – are used as injections into the affected area (in severe forms of the disease);
- Muscle relaxants – used to relax muscles, relieve pain and inflammation.
Massage for osteochondrosis

A massage course for osteochondrosis must be completed every six months. Therapeutic massage eliminates tension, relieves tension and improves blood circulation in the affected area. Only a doctor can say about the advisability of prescribing a massage; a prerequisite is remission of the disease.
Traction (spinal traction)
Artificial spinal traction is performed only under the supervision of medical personnel and with special equipment. High-quality traction allows you to evenly distribute the vertebrae in the spine. Pain, pinching and inflammation are reduced.
Manual therapy
Manual therapy for osteochondrosis of the spine is used to correct the curvature. The specialist exerts a targeted effect on the patient's muscular and skeletal system. After therapy, blood and lymph circulation improves, stiffness disappears and mobility occurs.
Physiotherapeutic treatment of osteochondrosis
It is only practiced during the remission phase of the disease; In the acute phase, this method of treatment is prohibited. Physiotherapy is used as an adjunctive therapy alongside medication. To relieve the symptoms of osteochondrosis, specialists use lasers, magnets and electricity (low frequency).
acupuncture

The basis of acupuncture is the correct effect on reflex zones and pain points. The therapy is prescribed only in conjunction with therapeutic massage to increase effectiveness. The therapy restores the possibility of natural loading of the spine without pain.
Exercise therapy for osteochondrosis
Physiotherapy is effective for all types of osteochondrosis and can be prescribed to patients of any age group. The type of exercises and the duration of their implementation are prescribed by the doctor. Moderate physical activity strengthens the back muscles, increases mobility and flexibility of the spine, and improves the patient's condition.
The patient can be prescribed the following types of courses: exercise therapy, therapeutic swimming, health path, mechanotherapy.
Important!Exercise therapy courses are contraindicated during periods of exacerbation of osteochondrosis!
Surgical treatment of osteochondrosis
For spinal osteochondrosis, surgery is rarely prescribed as the only treatment option. The human spine has a complex structure with many vertebrae and nerve endings that affect the coordinated functioning of the entire body. Surgery carries a high risk of complications, which is why it is only prescribed in the most difficult cases or when there is no improvement with other treatment methods.
Prevention of spinal osteochondrosis
Prevention is the best way to reduce the risk of osteochondrosis and achieve remission of existing spinal diseases. When carrying out preventive exercises, it is important to ensure that they are carried out regularly and only during the remission phase.
It is better to perform a gymnastic set of simple exercises at the same time. To avoid forgetting them, set a reminder on your cell phone or incorporate them into your morning hygiene rituals.
- Place your forehead on your palm and tense your neck muscles. Execution – 3 sets of 5-7 seconds each. Then repeat the same thing with the back of your head and the palm of your hand.
- The shoulder posture is straight, the head is straight. Slowly tilt your head to the right and then to the left as far as possible. Perform 5 times (slowly).
- Slowly tilt your head back slightly. Tighten your neck muscles and gradually move your chin towards your chest. Perform 5-7 times.
- Place your left palm near the left temple area (then right palm and right temple). Apply pressure to your palm, tensing your neck muscles. Execution – 3 times for 10 seconds.

Important!Don't rush when doing the exercises. Circular movements of the head are also prohibited because of the high risk of injury and pinched nerve endings.
The second set of preventive exercises for osteochondrosis can be performed at any time (especially after work or overexertion), but also regularly:
- Stand straight, feet together, arms relaxed, breathe deeply. Raise your arms up and exhale. Approach – 6-8 times.
- Lie relaxed on your stomach with your arms along your body. Bend up, put your hands down and try to lift your head and feet. Stay in this position for 5 seconds. Return to the starting position. Repeat – 5-7 times.
- Sit on a chair. Place your hands behind your head (take a deep breath), bend back 4-5 times so that your shoulder blades touch the back of the chair (exhale). Repeat – 5-7 times.
- Stand up, bend back, take a deep breath. Relax your arms, bend forward, slowly lower your head and shoulders - breathe out. Approach – 10 times.
- Get on all fours. Go ahead. Bend your back and stay in this position for 3-4 seconds. Return to the starting position and repeat the procedure 5-7 times.
How do you stand, lie and sit with osteochondrosis?
Knowledge of correct posture, which helps to evenly distribute the load across the entire spine, is necessary not only for patients with osteochondrosis, but for all people. By following simple rules, you will notice a significant improvement in your general well-being and relief on your back. In addition, you can protect your spine from many diseases with serious, painful symptoms.
How do you sit correctly?
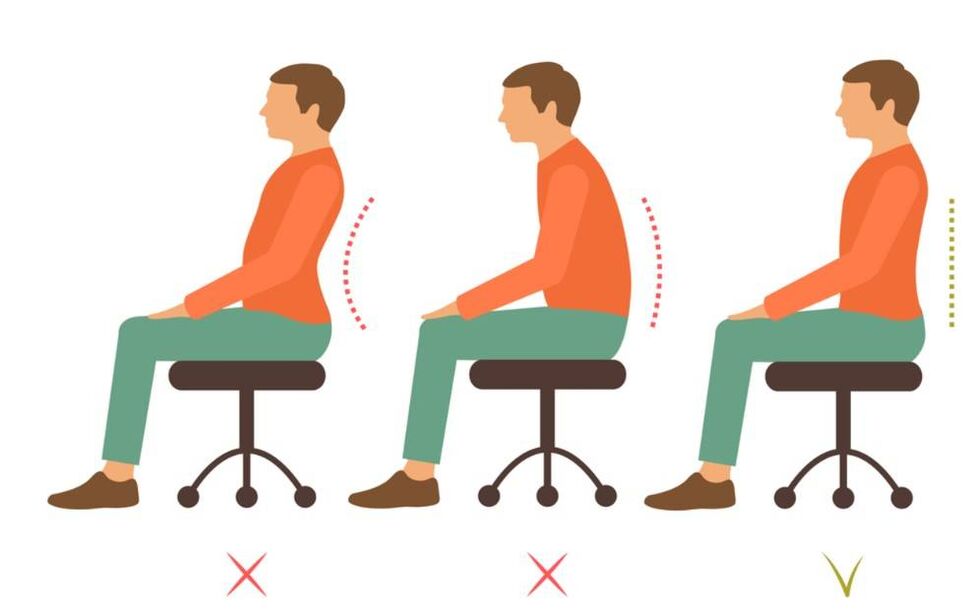
We learn to sit without squeezing, without provoking the risk of spinal deformation and the development of osteochondrosis:
- Criteria for choosing a chair/chair: seat depth - 2/3 of the hip length, seat height should correspond to the length of the lower leg. This way your feet will rest on the ground. Short people need to place a small step or bench under their feet;
- Pay attention to the depth of the work surface. It should be such that the legs do not need to be held to the sides or strongly bent;
- If you work for long periods while sitting, take a break every 20 minutes. Change the position of your legs, walk around, do light gymnastics;
- Sit behind the wheel with minimal stress. Your back should be against the seat; a small pillow or cushion between the chair and your lower back helps. If possible, get out of the car every 25-30 minutes to warm up;
- Heavily padded furniture is not good furniture for everyday use. To ensure an even load on the spine, the body must be supported on the ischial tuberosities, which is only possible when sitting on a medium-hard surface;
- Your back should always touch the back of your chair/work chair. Try to sit upright and avoid strong neck bends;
- Do not sit/lie in one position for a long time.
How do you stand correctly?
When a person stands in one position for a long time, a lot of stress is placed on the lumbar spine (and the entire spine), which negatively affects it. In order not to put too much strain on the spine and increase the risk of deformation, follow simple rules:
- Do not stand in one position for more than 10 minutes, change the position of your legs and arms.
- Relieve tension in the neck - tilt your head to the right and left, stretch your arms forward, bend your back forward and backward - relax your back and lower back;
- When you lift something from the floor, bend over, bend your knees, or squat, find a place to support your hands.
- move, walk short distances so as not to stand still;
- Try not to bend too much (back, head) when doing housework (cleaning, ironing, cooking). When cleaning low or hard-to-reach surfaces, get down on one knee.
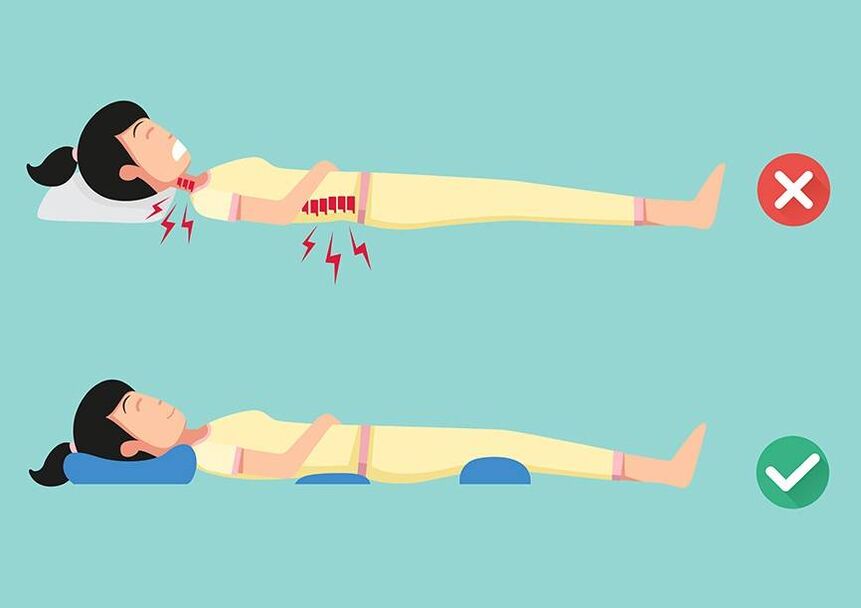
How do you lie down?
The ideal sleeping surface is a bed with a medium-firm mattress (ideally an orthopedic mattress that maintains the physiological curvatures of the spine). The bed should not be made of wood or too soft.
How do you lie down correctly when you are in severe pain?
- Back pain – lie on your stomach and place a small pillow under your lower back (so as not to increase the pain by bending over);
- Leg pain – place a pillow (made from a towel or blanket) under your knees. The pain syndrome will gradually subside;
- Neck pain – place your hand under your head or a pillow under your neck.
How to get out of bed in the morning during an attack of osteochondrosis?
- Perform a brief warm-up of the upper and lower extremities.
- change your position;
- Move from a lying position to a sitting position and grasp your leg with your hands bent at the knee.
- Lower your legs to the floor one at a time.
- Get up slowly, any sudden movement can increase the pain.
How do you lift and move weights correctly?
Improper lifting and carrying of heavy objects is one of the most common causes of hernias, osteochondrosis and bulges. Sharp lifting of weights is associated with a sudden "shooting" in various parts of the spine and the appearance of acute pain that lasts for a long time. Turning the body when carrying heavy objects is also prohibited.
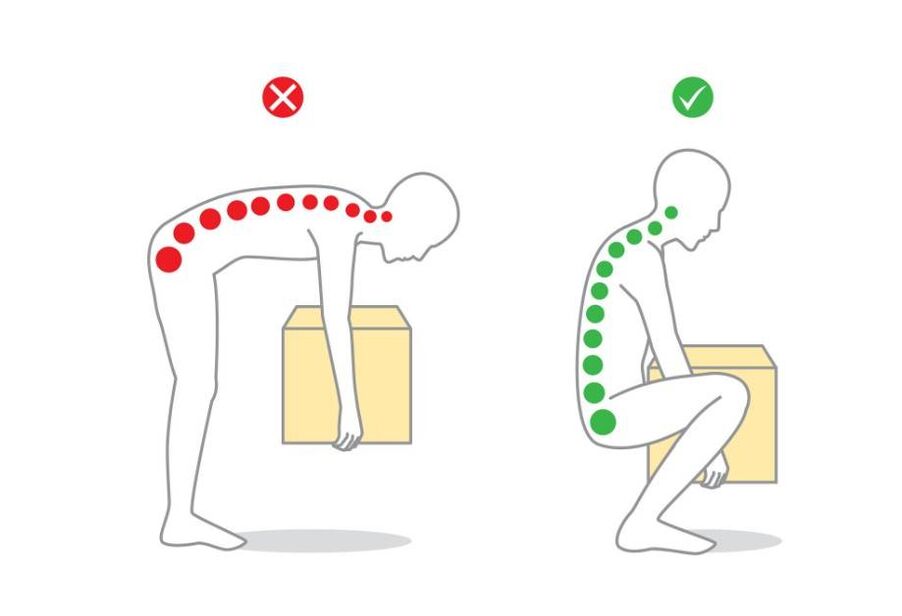
How do I lift a heavy object?
- Wear a wide belt.
- Crouch down. Keep your neck and back straight.
- Hold the object in place with both hands, slowly stand up and keep your back straight.
How do you move a heavy object?
- Distribute the load evenly between both hands, do not carry everything in one;
- If osteochondrosis is diagnosed, lifting weights over 15 kg is not recommended.
- Buy a backpack (an important requirement is an orthopedic back and wide straps). The advantages of a backpack are an even load on the spine + free hands;
- Do not lean forward or backward sharply.
Diploma
Osteochondrosis of the spine most often develops between the ages of 25 and 40. The risk group for morbidity includes people with a passive lifestyle who spend most of their time standing or in incorrect positions, putting a lot of strain on the spine. Osteochondrosis can be cured using conservative methods, provided that a specialist is consulted in a timely manner. In advanced cases, surgical intervention is used. Self-medication is contraindicated.
Regular preventive exercises will help relieve the symptoms of osteochondrosis, maintain the functionality of the spine and protect against deformation. If you neglect your health, the patient may delay visiting the doctor until hernias, paralysis and disability appear.
























